Real-Time, Prospective Cost Avoidance Solutions for Medicaid Payers
Payer of last resort providers are challenged with the difficult task of recovering payments when primary coverage information is not presented by the recipient at the time services are rendered. For a multitude of reasons, many recipients do not share other coverage information or are unaware that other coverage exists.
Without technology at the point of sale to prospectively identify other coverage, payer of last resort providers must accept claims and use manual pay and chase processes to retrospectively identify and track down primary payers for reimbursement. Unfortunately, these traditional recovery processes are inefficient, expensive and produce recovery rates of less than 17% of the dollars actually billed to primary payers.
ProTPL, a real-time point of sale cost avoidance service, was developed by Syrtis Solutions to support the cost avoidance and recovery needs of the payer of last resort market. The company’s founders, comprised of industry veterans with experience in pharmacy claims processing and claimant recovery processes, recognized that the market needed a technology-based solution to improve recovery.
ProTPL Proprietary Technology
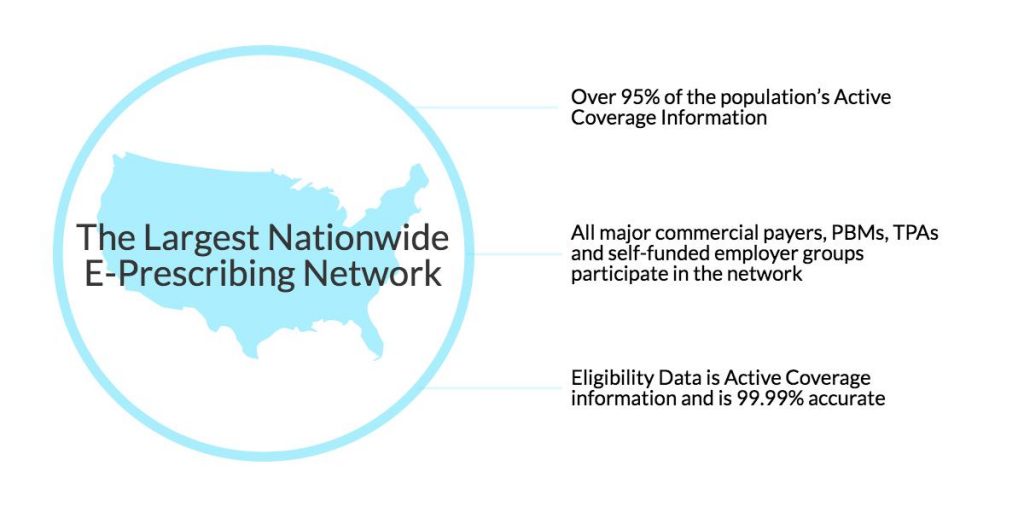
ProTPL accesses the nation’s largest E-Prescribing master patient index (MPI) utilizing industry standard transactions at the point of sale. The program has identified that between 6% – 14% of all claims submitted under payer of last resort health plans have other pharmacy coverage.
Integration of ProTPL results in the real-time identification of claims that have other coverage. These claims can be cost avoided along with all future claims for that recipient. This effectively eliminates the post-payment recovery process all together. In addition, the captured pharmacy information can be cross walked to the recipients active medical coverage information for added cost avoidance savings.
 As an additional benefit to payers, information obtained through the program can be used to identify and recover earlier pharmacy claims and used to discover other medical coverage information to support medical claims recovery efforts.
As an additional benefit to payers, information obtained through the program can be used to identify and recover earlier pharmacy claims and used to discover other medical coverage information to support medical claims recovery efforts.
Syrtis’ proprietary software processes transactions in sub-seconds through standard pharmacy transaction sets and is seamlessly integrated into any pharmacy program. ProTPL eliminates disruption for the provider and patient at the point of sale improving patient care and service.
ProTPL Process
ProTPL can be customized based on each payer’s unique needs. The daily claims file is automatically routed to the Syrtis Decision Support (SDS) system and queries Surescripts’ master patient index. When other health information is found, the system returns the corresponding coverage information that was identified. The identified coverage information is then available to be used by the customer for future cost avoidance.